L00-L99
Pressure Ulcer Stages
Codes from ICD-10-CM category L89 are combination
codes that identify the site of the pressure ulcer and the
stage of the ulcer.
ICD-10-CM classifies pressure ulcer stages based on
severity, which is designated by stages 1-4, unspecified stage and unstageable.
Assign as many codes from category L89 as needed to report all the pressure ulcers the patient has.
Unstageable Pressure Ulcers
Assignment of the ICD-10 CM codes for unstageable pressure ulcer (L89.--0)
is based on documentation. These codes
are used for pressure ulcers whose stage cannot be clinically
determined perhaps because the ulcer is covered by eschar or for some other reason and pressure ulcers that are
documented as deep tissue injury but not documented as due to
trauma.
Do not confuse "unstageable" pressure ulcer with "unspecified stage" when there is no documentation
regarding the stage of the pressure ulcer.
Documented Pressure Ulcer Stage
Assignment of the ICD-10-CM pressure ulcer stage code is based on documentation of the stage or documentation of the
terms found in the Alphabetic Index.
For clinical terms
describing the stage that are not found in the Alphabetic Index,
and there is no documentation of the stage, the provider should
be queried.
Healed Pressure Ulcers
No ICD-10-CM code is assigned if the documentation states that the pressure
ulcer is completely healed.
Healing Pressure Ulcers
Pressure ulcers documented as healing should be assigned the pressure ulcer stage code based on the
documentation in the medical record.
If the documentation does
not state the stage of the healing pressure
ulcer, assign the appropriate code for unspecified stage.
If the documentation is unclear as to whether there is a current (new) pressure ulcer or if there is a healing pressure ulcer, query the provider.
Pressure Ulcer Evolving
If a pressure ulcer at one stage progresses to a higher stage, then report the code for the highest stage for that site.
ICD-10-CM Official Guidelines for Coding and Reporting
Wednesday, November 11, 2015
Thursday, October 29, 2015
ICD-10-CM Dental Screening Codes
Screening Codes
Z01.20-Encounter for dental exam and cleaning without abnormal findings.
Z01.21-Encounter for dental exam and cleaning with abnormal findings
**********************************************************************
The Most Critical Rule In the Medical Coding World
************************************************************************
ICD-10-PCS CODING TIP
If multiple coronary artery sites are bypassed, a separate procedure code is required for each coronary artery site that uses a different device and/or qualifier.
ICD-10-PCS Official Guidelines for Coding and Reporting 2015
Screening Codes
Z01.20-Encounter for dental exam and cleaning without abnormal findings.
Z01.21-Encounter for dental exam and cleaning with abnormal findings
**********************************************************************
The Most Critical Rule In the Medical Coding World
Begin your search for the correct code assignment through the
Alphabetic Index. Never begin searching initially in the Tabular List as this
will lead to coding errors
************************************************************************
ICD-10-PCS CODING TIP
If multiple coronary artery sites are bypassed, a separate procedure code is required for each coronary artery site that uses a different device and/or qualifier.
ICD-10-PCS Official Guidelines for Coding and Reporting 2015
Monday, October 19, 2015
ICD-10-CM CODING TIP
First listed Z codes indicate:
• that a person with a resolving disease or injury or chronic is being seen for specific aftercare, such as the removal of internal fixation devices such as orthopedic pins
CODES
Z codes can be used in any health care setting and may be first-listed (principal diagnosis code in the inpatient setting) or
secondary code, depending on the circumstances of the encounter.
Certain Z codes may only be listed as first-listed or principal diagnosis. There are 20 of these first listed/principal Z codes and they are listed in your ICD-10-CM manual in the front of the book under the Official Guidelines for Coding and Reporting for Chapter 21-16.
• that a person with a resolving disease or injury or chronic is being seen for specific aftercare, such as the removal of internal fixation devices such as orthopedic pins
• that the patient is seen for the sole
purpose of special therapy, such as radiotherapy or chemotherapy.
• that a person not currently ill is
encountering the health service for a specific reason, such as to act as an
organ donor, to receive prophylactic care, or to receive counseling
• the birth status of newborns
Additional codes indicate:
• that a patient has a history, a health
status, or another problem that is not in itself an illness or injury but may
influence patient care.
Saturday, October 10, 2015
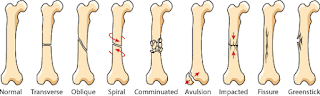
CODING FRACTURES IN ICD-10
ICD-10 & Orthopedic Coding
Documentation is the
for specificityDocumentation is the
- · Type of fracture (Open, closed, pathological, neoplastic disease, stress)
- · Pattern (Comminuted, oblique, segmental, spiral, transverse)
- · Etiology to document in the external cause codes
- · Encounter of care (Initial, subsequent, sequelae)
- · Healing status, if subsequent encounter (normal or delayed healing, nonunion, malunion)
- · Localization (Shaft, head, neck, distal, proximal, styloid)
- · Displacement (Displaced, non displaced)
- · Classification (Gustilo-Anderson, Salter-Harris)
- · Any complications, whether acute or delayed (Direct result of trauma sustained)
- · Intra-articular or extra-articular involvement ICD-10 Clinical Concepts
A fracture not documented as open or closed should be coded to closed.
A fracture not documented as displaced or not displaced should be
coded to displaced.
Traumatic fractures are coded using the appropriate 7th
character for initial encounter (A, B, C) while the patient is
receiving active treatment for the fracture. Examples of active
treatment are: surgical treatment, emergency department
encounter, and evaluation and treatment by a new physician.
The appropriate 7th character for initial encounter should also
be assigned for a patient who delayed seeking treatment for the
fracture or nonunion.
Fractures are coded using the appropriate 7th character for
subsequent care for encounters after the patient has completed
active treatment of the fracture and is receiving routine care for
the fracture during the healing or recovery phase. Examples of
fracture aftercare are: cast change or removal, removal of
external or internal fixation device, medication adjustment, and
follow-up visits following fracture treatment.
Care for complications of surgical treatment for fracture repairs
during the healing or recovery phase should be coded with the
appropriate complication codes.
Care of complications of fractures, such as malunion and
nonunion, should be reported with the appropriate 7th character
for subsequent care with nonunion (K, M, N,) or subsequent
care with malunion (P, Q, R)
The aftercare Z codes would not be used for aftercare for
traumatic fractures. For aftercare of a traumatic fracture, assign
the acute fracture code with the appropriate 7th character. ICD-10-CM Official Guidelines for Coding and Reporting
Saturday, October 3, 2015
WELL IT'S HERE..................
The Arrival of ICD-10
For several years, there was so much anticipation for ICD-10 like a roaring lion getting ready to attack. I went to bed about 10:00 PM on September 30, 2015 and work up at 6:00 AM on October 1, 2015 to meet a calm lamb. Not sure if this is the calm before the storm, time will tell. Everyone is just getting started so not sure how it will go.
How to Proceed
So in the mean time, stay calm and forge ahead, you got this! Remember the basics of coding:
ICD-10-CM Coding Tip
Aftercare visit codes cover situations when the initial treatment of a disease has been performed and the patient requires continued care during the healing or recovery phase, or for the long-term consequences of the disease. The aftercare Z code should not be used if treatment is directed at a current, acute disease. The diagnosis code is to be used in these cases. Exceptions to this rule are codes Z51.0, Encounter for antineoplastic radiation therapy, and codes from subcategory Z51.1, Encounter for antineoplastic chemotherapy and immunotherapy. The aftercare Z codes should also not be used for aftercare for injuries. For aftercare of an injury, assign the acute injury code with the appropriate 7th character (for subsequent encounter). The aftercare codes are generally first-listed to explain the specific reason for the encounter. An aftercare code may be used as an additional code when some type of aftercare is provided in addition to the reason for admission and no diagnosis code is applicable. Aftercare codes should be used in conjunction with other aftercare codes or diagnosis codes to provide better detail on the specifics of an aftercare encounter visit, unless otherwise directed by the classification.
ICD-10-CM Official Guidelines for Coding and Reporting
For several years, there was so much anticipation for ICD-10 like a roaring lion getting ready to attack. I went to bed about 10:00 PM on September 30, 2015 and work up at 6:00 AM on October 1, 2015 to meet a calm lamb. Not sure if this is the calm before the storm, time will tell. Everyone is just getting started so not sure how it will go.
How to Proceed
So in the mean time, stay calm and forge ahead, you got this! Remember the basics of coding:
- Review the documentation
- Abstract the information needed to select the correct diagnosis and procedure code
- Determine the "reason" for the encounter
- Determine the procedure performed
- Start with the index of the coding book
- Look up the term
- Make notes of the recommended codes
- Go to the Tabular for ICD or the main part of the CPT book
- Review the codes
- Read all notes, instructions, section guidelines
- Review any additional references such as coding guidelines, Coding Clinic, CPT Assistant or Coder's Desk Reference to select the correct code
- Link the codes correctly
- If applicable, apply modifiers
Sound familiar?
ICD-10-CM Coding Tip
Aftercare visit codes cover situations when the initial treatment of a disease has been performed and the patient requires continued care during the healing or recovery phase, or for the long-term consequences of the disease. The aftercare Z code should not be used if treatment is directed at a current, acute disease. The diagnosis code is to be used in these cases. Exceptions to this rule are codes Z51.0, Encounter for antineoplastic radiation therapy, and codes from subcategory Z51.1, Encounter for antineoplastic chemotherapy and immunotherapy. The aftercare Z codes should also not be used for aftercare for injuries. For aftercare of an injury, assign the acute injury code with the appropriate 7th character (for subsequent encounter). The aftercare codes are generally first-listed to explain the specific reason for the encounter. An aftercare code may be used as an additional code when some type of aftercare is provided in addition to the reason for admission and no diagnosis code is applicable. Aftercare codes should be used in conjunction with other aftercare codes or diagnosis codes to provide better detail on the specifics of an aftercare encounter visit, unless otherwise directed by the classification.
ICD-10-CM Official Guidelines for Coding and Reporting
Wednesday, September 30, 2015
Medical Necessity & Medical Coders
Medical necessity, what is it?
CMS defines medical necessity/medical necessary as "
It Is Not the Medical Coder's Responsibility......
It is not the responsibility of the medical coder to make up a diagnosis to meet medical necessity, however, it is the responsibility of the medical coder to verify the diagnosis, select the correct code to he highest level of specificity, follow Coding Guidelines, follow coding instructions in the ICD-CM Tabular, use all available resources, and link the ICD-CM code to the CPT code correctly.
The Responsibility of Establishing Medical Necessity Belongs to the Ordering Provider
Documentation supporting the medical necessity such as diagnosis or procedure codes must be submitted with each claim. Without such evidence, the claim will be denied as being not medically necessary. The medical record must include documentation of the signs, symptoms, and conditions associated with the billed diagnosis and procedure codes. Documentation
Remember--
If it is not documented, it was not done
"Medical necessity of a service is the overarching criterion for payment in addition to the individual requirements of a CPT code. It would not be medically necessary or appropriate to bill a higher level of evaluation and management service when a lower level of service is warranted. The volume of documentation should not be the primary influence upon which a specific level of service is billed. Documentation should support the level of service reported. The service should be documented during, or as soon as practicable after it is provided in order to maintain an accurate medical record."CMS & MEDICAL NECESSITY
CMS defines medical necessity/medical necessary as "
| "Services or supplies that: are proper and needed for the diagnosis or treatment of your medical condition, are provided for the diagnosis, direct care, and treatment of your medical condition, meet the standards of good medical practice in the local area, and aren't mainly for the convenience of you or your doctor." Definition Medical Necessity |
It Is Not the Medical Coder's Responsibility......
It is not the responsibility of the medical coder to make up a diagnosis to meet medical necessity, however, it is the responsibility of the medical coder to verify the diagnosis, select the correct code to he highest level of specificity, follow Coding Guidelines, follow coding instructions in the ICD-CM Tabular, use all available resources, and link the ICD-CM code to the CPT code correctly.
The Responsibility of Establishing Medical Necessity Belongs to the Ordering Provider
Documentation supporting the medical necessity such as diagnosis or procedure codes must be submitted with each claim. Without such evidence, the claim will be denied as being not medically necessary. The medical record must include documentation of the signs, symptoms, and conditions associated with the billed diagnosis and procedure codes. Documentation
Remember--
If it is not documented, it was not done
"Medical necessity of a service is the overarching criterion for payment in addition to the individual requirements of a CPT code. It would not be medically necessary or appropriate to bill a higher level of evaluation and management service when a lower level of service is warranted. The volume of documentation should not be the primary influence upon which a specific level of service is billed. Documentation should support the level of service reported. The service should be documented during, or as soon as practicable after it is provided in order to maintain an accurate medical record."CMS & MEDICAL NECESSITY
Sunday, September 27, 2015
Evaluation & Management (E/M) Coding Overview
The Story Behind Evaluation & Management CPT Codes
Today, we have over 38
pages of Evaluation and Management codes in our CPT Manual, well it was not always that way, in 1991, there
was a simple medical billing system that included levels of evaluation and
management medical services that took up only four pages in the CPT Manual.
In 1992, the Health Care
Financing Administration (HCFA),
mandated by congress, introduced a new, and complicated set of
physician billing codes. In May 1997, the version of the Documentation
Guidelines for Evaluation & Management Services included 54 pages covering patient history, clinical exam, family history, decision
complexity, body areas, organ systems, physical exam types, diagnostic tests,
and management options.
There are two different
sets of Evaluation and Management guidelines; 1995 and 1997. The 1997
guidelines were introduced by the Centers for Medicare
& Medicaid Services (CMS) to address some of
the problems that were found with the 1995 guidelines at the time.
The main difference between the two guidelines is in the examination part of the evaluation and management service.
Evaluation and
Management CPT Codes are a medical
billing system that healthcare providers
in the United States use so that they are able to be reimbursed by private insurance
companies and other payers such as Medicare and Medicaid.
Instructions for
Selecting a Level of E/M Service
The CPT codes in the Evaluation &
Management section are 99201-99499. The Evaluation and Management section is
the first section in the CPT Manual.
There are categories and subcategories to the Evaluation and Management codes.
In the Current
Procedural Terminology (CPT®) Manual, the following
instructions are found:
- Review the instructions for the selected category or
subcategory.
- Review the level of E/M
Service Descriptors & examples in the selected category or
subcategory.
- Determine the extent of history obtained.
- Determine the extent
of examination performed.
- Determine the Complexity of medical decision making.
Key Components
There are three key components in choosing an evaluation and management code. The history, examination, and medical decision making.
- Select the appropriate level of E/M service based on all
the key components for initial hospital care, office
consultation, initial inpatient consultation, office new patient, hospital
observation, emergency department, initial nursing facility
care, domiciliary care, new patient & home new patient.
- OR
- Select the appropriate level of E/M service based on two
of the three components for
office established, subsequent hospital;
care, subsequent nursing facility
care, domiciliary care established, & home established
patient.
- OR
- Select the appropriate level of E/M when counseling
and/or coordination of care dominates (more than 50%) the encounter with
the patient and/or family (face-to-face in the office or other outpatient
setting or floor/unit time in the hospital or nursing facility) then time shall
be considered the key or
controlling factor to qualify for a particular level of E/M
services.
Want to read more?
Medical Necessity
"Medical necessity of a service is the overarching criterion for payment in addition to the
individual requirements of a CPT code. It would not be medically necessary or
appropriate to bill a higher level of evaluation and management service when a lower
level of service is warranted. The volume of documentation should not be the primary
influence upon which a specific level of service is billed. Documentation should support
the level of service reported. The service should be documented during, or as soon as
practicable after it is provided in order to maintain an accurate medical record."CMS & MEDICAL NECESSITY
In future post, I will expand upon evaluation and management coding.
ICD-10-CM-Highlight
V97.33XD-Sucked into jet engine, subsequent encounter
Funny
Statistically…. 9 out of 10 injections are in vein.”
Subscribe to:
Posts (Atom)